Informed consent is a cornerstone of medical ethics and plays a vital role in nursing practice. It ensures patients are fully informed about procedures, treatments, or interventions, while guaranteeing their participation is voluntary. Understanding informed consent empowers nurses to advocate for patients’ rights, promote autonomy, and maintain trust in healthcare settings.
What is Informed Consent?
Informed consent is a communicative process between healthcare professionals and patients. It involves providing clear, relevant information about proposed care, including risks, benefits, and alternatives. Patients are given the opportunity to ask questions, consider their options, and voluntarily accept or decline the recommended treatment.
Ethical Principles Guiding Informed Consent
- Autonomy: Respecting patients’ independence to make decisions about their care based on personal values and beliefs.
- Beneficence: Ensuring patients receive necessary information to support their well-being.
- Non-Maleficence: Informing patients of potential risks to help avoid harm.
- Justice: Seeking consent fairly, ensuring all patients receive equitable care regardless of background.
Steps in the Informed Consent Process
- Disclosure: Communicate relevant details regarding diagnosis, treatment options, and associated risks.
- Comprehension: Confirm patient understanding using clear language and addressing literacy or cultural barriers.
- Voluntariness: Ensure the decision is made freely, without coercion or pressure.
- Competency: Assess the patient’s capacity to make informed choices.
- Documentation: Properly record the discussion and the patient’s decision.
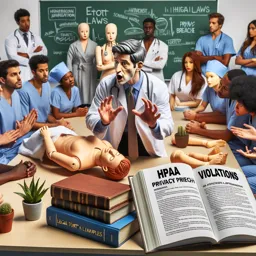
Nurses’ Role in Supporting Informed Consent
Nurses act as advocates, clarifying information, addressing concerns, and protecting vulnerable patients. When patients lack capacity, nurses help identify appropriate surrogates or legal representatives to ensure ethical care.
Overcoming Challenges
Barriers such as language differences, cultural beliefs, or limited health literacy can complicate informed consent. Strategies include using interpreters, cultural mediators, visual aids, and maintaining a patient-centered approach throughout the process.
Conclusion
Mastering informed consent principles is essential for nurses to provide ethical and effective care. By championing informed consent, nurses uphold professional responsibilities, foster patient trust, and empower individuals in their healthcare decisions.