Why Scenario Walkthroughs and Quick-Reference Tables Matter
In real-life child emergencies, the hardest part is often not knowing what to do—it is doing the right thing quickly while stress, noise, and competing demands pull your attention away. Scenario walkthroughs and quick-reference warning sign tables are tools that reduce decision fatigue. They help you translate knowledge into action by giving you a rehearsed sequence (walkthrough) and a fast “pattern match” list (table) for when you are unsure how serious something is.
This chapter focuses on how to use these tools in home, school, and everyday settings without re-teaching the detailed first aid techniques already covered elsewhere. The goal is to help you organize your response: what to notice, what to do first, what to document, what to monitor, and when to escalate.
Two complementary tools
Scenario walkthroughs are short, realistic stories with a step-by-step response. They train your brain to recognize a situation, take control of the environment, and follow a sequence under pressure.
Quick-reference warning sign tables are compact checklists that highlight “this is not normal” signs. They are designed to be scanned in seconds and used repeatedly.
How to Use a Scenario Walkthrough (A Repeatable Template)
Use the same structure each time so it becomes automatic. You can print this as a one-page sheet for a first aid binder.
- Listen to the audio with the screen off.
- Earn a certificate upon completion.
- Over 5000 courses for you to explore!
Download the app
Template: S-C-A-N (Scene, Child, Actions, Next)

Scene: What is happening around you? What hazards must be controlled (traffic, water, electricity, crowd, sharp objects)? Who can help (another adult, staff, older teen)?
Child: What is the child doing right now (walking, crying, silent, sleepy, struggling to breathe)? What is the main complaint? What changed from baseline?
Actions: The first 3–5 things you will do in order. Keep them simple: position, comfort, protect, retrieve supplies, start timing, notify.
Next: Monitoring and escalation plan. What will you re-check? What will trigger urgent care or emergency response? Who needs to be informed (parent/guardian, school nurse, coach)? What documentation is needed?
When you practice, say the steps out loud. In real events, speaking your plan helps you stay organized and directs bystanders: “You call the office. You bring the first aid kit. I’m staying with the child.”
Scenario Walkthroughs (Home, School, and Everyday Emergencies)
Scenario 1: Playground collision with delayed symptoms
Scene: Two children collide while running. One sits down, looks stunned, then says they are “fine” and wants to keep playing. Teachers are supervising; other children crowd in.

Child: Child is upright, talking, but quieter than usual. No obvious bleeding. They report a headache “starting now.”
Actions (step-by-step):
Move the child to a quieter area with an adult staying close; reduce stimulation and crowding.
Do a quick check for visible injury and comfort positioning. Start a timer or note the time of impact.
Ask simple, baseline questions: “What happened?” “Where are you?” “What hurts?” Note any confusion or repeated questions.
Notify the designated school contact (nurse/office) and the parent/guardian per policy, even if symptoms seem mild.
Set a monitoring plan for the next 1–2 hours: check behavior, headache, nausea, balance, and alertness at regular intervals.
Next: Use the head-injury warning sign table below to decide whether to escalate immediately or continue observation with parent pickup. Document: time, mechanism (collision), initial symptoms, and changes over time.
Scenario 2: Toddler with sudden limp after a fall at home
Scene: A toddler trips over a toy and falls. They cry hard, then calm, but now refuse to put weight on one leg. No obvious deformity.
Child: Alert, clingy, points to ankle/knee area but cannot describe well.
Actions (step-by-step):
Keep the child still and comfortable in a caregiver’s lap; avoid repeated “try walking” tests.
Expose the area gently (remove shoe/sock if tolerated) and compare both sides for swelling, bruising, or unusual position.
Use simple support: keep the limb in the position found; apply a cold pack wrapped in cloth if swelling is present and the child tolerates it.
Plan transport: if the child cannot bear weight or pain is significant, arrange same-day medical evaluation.
Prepare information: exact time, fall height, what the child landed on, and what changed afterward (refusal to bear weight).
Next: Use the limb injury warning sign table to decide whether urgent evaluation is needed (for example, severe pain, deformity, numbness, or inability to use the limb). Document what you observed before swelling increases.
Scenario 3: School bathroom—possible fainting vs. “just tired”
Scene: A student is found sitting on the bathroom floor, pale and sweaty. Another student says, “They almost passed out.”
Child: Teen is awake but slow to respond, says they feel dizzy and nauseated.
Actions (step-by-step):
Get help immediately (send a runner to the office/nurse). Stay with the student; ensure privacy and safety.
Position for safety: seated or lying down to prevent a fall. Loosen tight clothing if appropriate.
Ask targeted questions: recent illness, skipped meals, new medications, pain, heavy menstrual bleeding, diabetes history, pregnancy possibility (if appropriate and per policy), substance exposure.
Check for injuries from any fall and note mental status: are they oriented, speaking clearly, able to follow commands?
Do not allow the student to stand quickly; reassess after a few minutes.
Next: Use the “altered behavior/alertness” and “chest pain/breathing” warning sign tables. Escalate if symptoms persist, recur, or include chest pain, severe headache, shortness of breath, or confusion. Document: time found, witness report, position, and symptom progression.
Scenario 4: After a pool party—child seems fine, then develops cough later
Scene: A child swallowed water during swimming, coughed a lot, then returned to playing. Hours later at home, they develop persistent coughing and seem unusually tired.

Child: Awake, but coughing more than expected; caregiver notes “not acting like themselves.”
Actions (step-by-step):
Stop activity and keep the child calm; observe breathing effort and ability to speak in full sentences.
Check for worsening signs: fast breathing, chest retractions, bluish lips, unusual sleepiness, or repeated vomiting.
Note the timeline: when the water incident happened, when coughing started again, and whether symptoms are increasing.
Contact medical advice line/urgent care for guidance if symptoms persist or increase; escalate urgently if breathing difficulty appears.
Keep the child under close supervision; avoid sending them to sleep unsupervised if symptoms are evolving.
Next: Use the breathing warning sign table. The key is change over time: a delayed increase in cough, breathing effort, or unusual drowsiness after a water event warrants prompt evaluation.
Scenario 5: Field trip—unknown rash spreading quickly
Scene: On a field trip, a child develops hives on the neck and arms. They are anxious and scratching. You do not have their full medical history immediately available.
Child: Talking, no obvious breathing distress, but rash is spreading over minutes.
Actions (step-by-step):
Stop exposure if suspected (move away from plants/animals/food area). Keep the child with a calm adult.
Ask about known allergies and whether they carry medication; check the trip medical forms if available.
Assign tasks: one adult stays with the child; another retrieves the first aid kit and contacts the trip lead/school nurse.
Monitor for escalation signs: voice change, coughing, swelling of lips/tongue, vomiting, dizziness, or breathing difficulty.
Communicate early with parents/guardians and follow the child’s action plan if one exists.
Next: Use the allergy/anaphylaxis warning sign table to decide if this is “skin-only” or progressing. Document suspected trigger, time of onset, and changes every few minutes.
Scenario 6: Kitchen incident—possible ingestion, caregiver unsure what was swallowed
Scene: A caregiver finds an open bottle of household product and a toddler with wet lips. The caregiver is unsure if the child swallowed any.

Child: Awake, drooling slightly, fussy. No clear symptoms yet.
Actions (step-by-step):
Remove the product from reach and keep the container for identification; do not induce vomiting or give “neutralizing” drinks unless instructed by professionals.
Wipe the child’s mouth/face gently; remove contaminated clothing if needed and rinse skin/eyes if exposed.
Call the appropriate poison guidance resource immediately with the product name, ingredients (if listed), and estimated amount/time.
Observe for red flags: trouble swallowing, persistent vomiting, coughing, lethargy, or breathing difficulty.
Prepare for transport if advised; bring the container and any remaining product.
Next: Use the ingestion warning sign table. The key decision is not “wait and see” when the substance is unknown or potentially caustic; get expert guidance early.
Quick-Reference Warning Sign Tables (Scan-and-Decide)
These tables are designed for quick scanning. They do not replace local protocols or a clinician’s judgment. Use them to decide whether you should: (1) continue close observation, (2) seek same-day evaluation, or (3) activate emergency response.
Table 1: Breathing and Oxygenation Warning Signs
LOOK FOR (any one can be serious) WHAT IT MAY MEAN WHAT TO DO NEXT (high level) -------------------------------------------------------------------------------------------------------------------------------- Struggling to breathe, gasping, cannot Not enough air moving Escalate urgently; keep child calm and upright if tolerated speak/cry normally Blue/gray lips or face, very pale/ashen Low oxygen Emergency response Chest retractions, nostril flaring, Increased work of breathing Same-day urgent evaluation; escalate if worsening head bobbing (infants) Noisy breathing with drooling or Airway swelling/obstruction risk Emergency response inability to swallow Breathing gets worse over minutes, Deterioration Escalate; do not leave child unattended especially after water event or illness Child becomes unusually sleepy or hard Oxygen/brain perfusion concern Emergency response to wake along with breathing symptomsTable 2: Alertness and Behavior Warning Signs
LOOK FOR WHY IT MATTERS WHAT TO DO NEXT (high level) -------------------------------------------------------------------------------------------------------------------------------- Child is difficult to wake, unusually Possible serious illness/injury Emergency response floppy, or not interacting Confusion, repeated questions, Brain involvement or medical issue Same-day urgent evaluation; escalate if worsening disorientation, or behavior far from baseline Fainting with persistent symptoms Ongoing perfusion problem Urgent evaluation; emergency response if chest pain/breathing issues New weakness, trouble walking, Neurologic concern Emergency response slurred speech, or one-sided changes Persistent inconsolable crying in infant Pain or serious illness Same-day evaluation; urgent if paired with fever, lethargy, or swellingTable 3: Bleeding and Circulation Warning Signs
LOOK FOR WHY IT MATTERS WHAT TO DO NEXT (high level) -------------------------------------------------------------------------------------------------------------------------------- Bleeding that will not stop with steady Risk of significant blood loss Emergency response or urgent care depending on severity pressure Blood soaking through dressings rapidly Ongoing hemorrhage Emergency response Signs of shock (very pale, clammy, Poor circulation Emergency response weak, dizzy, fast breathing) Vomiting blood or coughing blood Internal bleeding concern Emergency response Large swelling that is rapidly expanding Possible internal bleeding Urgent evaluationTable 4: Head/Neck/Spine “Do Not Ignore” Signs
LOOK FOR WHY IT MATTERS WHAT TO DO NEXT (high level) -------------------------------------------------------------------------------------------------------------------------------- Neck pain after trauma, inability to Possible spinal injury Emergency response; minimize movement move neck normally Worsening headache, repeated vomiting, Possible brain injury Emergency response or urgent evaluation per severity increasing confusion, or unusual drowsiness Seizure after head injury Brain irritation/bleeding concern Emergency response Unequal pupils, vision changes, Neurologic red flag Emergency response weakness, or trouble speakingTable 5: Abdominal and Genital/Urinary Warning Signs
LOOK FOR WHY IT MATTERS WHAT TO DO NEXT (high level) -------------------------------------------------------------------------------------------------------------------------------- Severe abdominal pain that is worsening, Surgical/serious illness concern Same-day urgent evaluation; emergency response if severe or with shock signs rigid belly, or pain with movement Abdominal pain with persistent vomiting, Dehydration/obstruction concern Same-day evaluation green vomit, or blood in vomit/stool Testicular pain/swelling in boys/teens Time-sensitive emergency Emergency evaluation Painful urination with fever, flank pain, Kidney infection concern Same-day evaluation or child appears very illTable 6: Skin, Allergy, and Infection Warning Signs
LOOK FOR WHY IT MATTERS WHAT TO DO NEXT (high level) -------------------------------------------------------------------------------------------------------------------------------- Hives plus breathing symptoms, vomiting, Anaphylaxis risk Emergency response; follow action plan dizziness, or swelling of lips/tongue Rash that does not blanch (purple/red Possible serious infection/bleeding Emergency response spots), especially with fever or lethargy Rapidly spreading redness with fever, Serious skin infection concern Same-day urgent evaluation severe pain, or child appears very ill Swelling of face/eyes with fever or Airway/eye risk Urgent evaluation; emergency response if breathing affected trouble swallowingTable 7: Ingestion/Poisoning Warning Signs
LOOK FOR WHY IT MATTERS WHAT TO DO NEXT (high level) -------------------------------------------------------------------------------------------------------------------------------- Unknown substance, caustic product High risk even without symptoms Call poison guidance immediately; emergency response if symptoms (drain cleaner, strong acids/alkalis) Trouble swallowing, drooling, burns Airway/esophagus injury risk Emergency response around mouth Persistent vomiting, severe abdominal pain, Systemic toxicity Emergency response or urgent evaluation per guidance confusion, seizures Medication ingestion where dose is unknown Potential overdose Call poison guidance immediately; do not wait for symptomsBuilding Your Own Quick-Reference Pack (Home and School)
A quick-reference pack is only useful if it matches your environment and is easy to access. Build it like a “grab-and-go” resource.
What to include (and how to format it)
One-page warning sign tables: Print the tables above in large font. Use bold headings and keep each table to one page.
Scenario cards: Create 6–10 cards for your most likely situations (playground injuries, sports practice, bath time, kitchen incidents, field trips). Each card follows the S-C-A-N template.
Contact sheet: Emergency numbers, poison guidance resource, pediatrician, parent/guardian contacts, and school escalation chain. Keep it laminated.
Documentation mini-form: A half-page form to record time, symptoms, actions taken, and who was notified. This reduces memory errors during stress.
Example: Documentation mini-form (copy/paste)
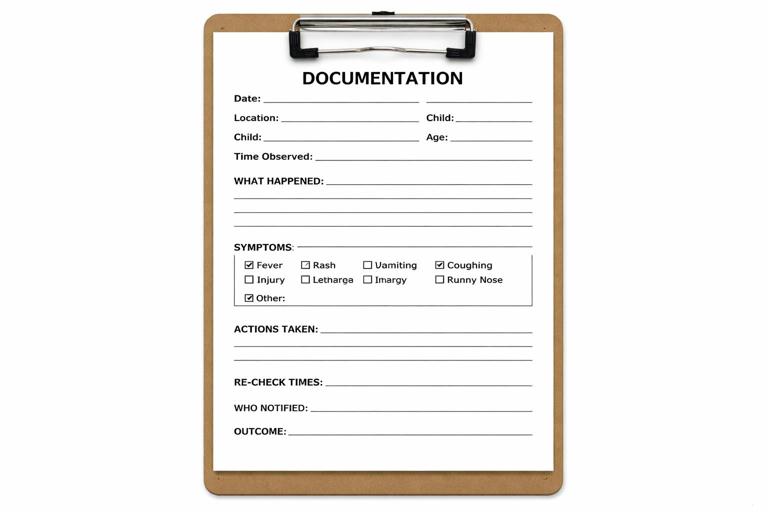
Date: ________ Location: ________ Child: ________ Age: ________ Time event started/observed: ________ What happened (mechanism/exposure): __________________________________________ Symptoms observed (circle): breathing trouble / rash / vomiting / pain / bleeding / behavior change / other: ________ Actions taken: ______________________________________________________________ Times re-checked and changes: ______________________________________________ Who notified (time): parent/guardian ________ nurse/office ________ emergency services ________ Outcome/next step: __________________________________________________________Practice Method: Turn Walkthroughs into “If-Then” Habits
To make these tools usable under stress, practice converting them into short if-then statements. This is not about memorizing medical details; it is about rehearsing your first minute.
Examples of if-then statements
If a child looks “not like themselves” after an impact, then I move them to a quiet area, note the time, notify the designated contact, and start scheduled re-checks.
If a child’s breathing looks harder than normal, then I stop activity, position for easier breathing, assign someone to call for help, and watch for the breathing warning signs.
If I suspect ingestion and I am not sure what it was, then I secure the container, call poison guidance immediately, and monitor for swallowing/breathing changes.
Adapting Scenarios to Different Settings
Home: fewer helpers, faster access to history
At home you often know the child’s baseline and medical history, but you may be alone. Your scenario cards should emphasize: controlling hazards (stove, bath, stairs), keeping siblings safe, and having a “call list” ready. Place the quick-reference tables near the first aid kit and in the kitchen.
School/childcare: more helpers, more communication steps
In schools, the challenge is coordination and documentation. Your scenario cards should include: who retrieves the kit, who manages the class, who contacts the nurse/office, and how to reach parents. Keep the warning sign tables in the nurse’s office and in a substitute folder.
Sports/field trips: delayed access to supplies
For trips, reduce your pack to essentials: warning sign tables, contact sheet, documentation form, and any child-specific action plans. Scenario cards should emphasize: staying with the child, delegating to another adult, and tracking time and symptom progression until help arrives.