Why “mindset” matters in pediatric first aid
Pediatric first aid is not only a set of techniques; it is a way of thinking under pressure. Children and infants can deteriorate faster than adults, symptoms can be subtle, and caregivers often face strong emotions (fear, guilt, urgency). A good first aid mindset helps you act early, avoid common traps (waiting too long, doing too much, or doing the wrong thing), and make decisions that are safe, simple, and appropriate for your training level.
This chapter focuses on three pillars: (1) a pediatric first aid mindset that prioritizes safety and early recognition, (2) understanding your limits and the limits of first aid, and (3) decision pathways you can use at home, school, or in everyday settings to decide what to do next.
The pediatric first aid mindset
1) Safety first: you cannot help if you become the second patient
Before approaching a child, quickly scan for hazards: traffic, aggressive animals, electricity, water, fire/smoke, unstable furniture, broken glass, chemicals, or an unsafe crowd. In schools and public spaces, also consider infection risk and the need for protective barriers (gloves, mask if available) when there is blood or body fluids.
Practical example: A toddler is crying near a fallen shelf. Your first action is not to lift the child; it is to ensure the shelf is stable and won’t fall again, and to move other children away so you can work.

2) “Calm is a skill”: regulate yourself to regulate the child
Children read adult cues. If you look panicked, they often become more distressed, which can worsen breathing problems, bleeding control, and cooperation. Use a simple self-regulation routine: stop, take one slow breath, and speak in short, confident sentences. Assign tasks to bystanders to reduce your cognitive load.
- Listen to the audio with the screen off.
- Earn a certificate upon completion.
- Over 5000 courses for you to explore!
Download the app
- Use names: “Maya, I’m here. I’m going to help you.”
- Use one-step instructions: “Look at me. Breathe with me.”
- Use tasking: “You in the blue shirt, call emergency services now. You, bring the first aid kit.”
3) Think in patterns: children often show “general unwellness” before clear symptoms
Adults may describe symptoms precisely; children may not. Your mindset should prioritize observation: behavior, breathing, skin color, interaction, and movement. A child who is “not acting right” deserves attention even if you cannot name the problem.
Practical example: A child at school says “my tummy hurts,” but you notice they are unusually quiet, pale, and breathing faster than normal. Your mindset should treat this as potentially serious and trigger a structured assessment and decision pathway rather than assuming it is minor.
4) Early escalation is not failure
Many caregivers hesitate to call for help because they fear overreacting. In pediatric emergencies, calling early can be the safest choice. Your goal is not to “handle it alone,” but to get the child the right level of care at the right time. If you are unsure, use decision pathways that favor safety.
5) Do the most important things first
Under stress, people may focus on visible injuries (a cut, a bruise) and miss life threats (breathing trouble, altered consciousness). Train your mindset to prioritize what can kill quickly: airway, breathing, circulation, severe bleeding, and rapidly worsening mental status. This is not about memorizing a script; it is about ordering your attention.
Limits: what first aid can and cannot do
Scope of first aid
First aid is immediate, temporary care until professional help is available or the child is stable enough for routine care. It focuses on preventing worsening, supporting basic functions, and recognizing when escalation is needed. It does not replace diagnosis, prescriptions, imaging, or definitive treatment.
Your personal limits
Your limits are defined by training, available equipment, environment, and your ability to stay safe. A helpful mindset is to ask: “What is the safest effective action I can take right now with what I have?”
- Training limit: If you have not been trained to perform a procedure, do not improvise it in a child.
- Equipment limit: If you do not have the right tools (for example, a proper splint), focus on stabilization and comfort rather than complex immobilization.
- Environment limit: In a crowded playground, your priority may be moving the child to a safer area and controlling hazards.
- Emotional limit: If you feel overwhelmed, delegate and simplify: call for help, keep the child warm, monitor breathing, and stay with them.
Common “overhelping” traps
Overhelping can cause harm. Watch for these traps:
- Doing too many interventions: Repeatedly moving a child, forcing food or drink, or attempting multiple unneeded checks can worsen injuries or choking risk.
- Chasing a perfect diagnosis: First aid is about recognizing severity and supporting the child, not naming the exact condition.
- Delaying escalation: Waiting for symptoms to “prove” seriousness can waste critical time.
- Ignoring your own safety: Entering water, traffic, or an unsafe building without support can create additional victims.
What “monitoring” really means
Monitoring is an active skill. It means you repeatedly reassess key signs and note trends. In children, trends matter: a child who is getting sleepier, breathing faster, or becoming paler is often worsening even if they are still awake.
Practical monitoring checklist (repeat every few minutes if concerned):
- Breathing: rate, effort, sounds, ability to speak/cry
- Color: pink, pale, bluish, mottled
- Behavior: alert, responsive, confused, unusually sleepy
- Circulation: warmth of skin, sweating, obvious bleeding
- Pain: increasing, decreasing, or unchanged
Decision pathways: a structured way to choose your next action
Decision pathways reduce panic and help you avoid missing critical steps. They are not rigid rules; they are guides that prioritize safety and early escalation. Use them in any setting: home, school, sports, travel, or public spaces.
Pathway 1: The “Stop–Check–Act–Recheck” loop
This loop keeps you from freezing or rushing.
- Stop: Pause for one breath. Look for hazards. Decide who will call for help.
- Check: Rapidly assess responsiveness, breathing, and obvious severe bleeding. Look for signs of severe illness or injury.
- Act: Do the simplest high-impact action you can: call emergency services, control severe bleeding, position for comfort, keep warm, monitor.
- Recheck: Reassess frequently. If worsening, escalate.
Practical example: A child falls from a swing and is crying. You stop and scan for hazards, check responsiveness and breathing, look for severe bleeding, act by keeping them still and comfortable, and recheck for increasing sleepiness, vomiting, or worsening pain.

Pathway 2: “Red flags” that trigger emergency response
When any red flag is present, treat it as an emergency and seek urgent help. Red flags are about risk, not certainty.
- Unresponsive or difficult to wake
- Breathing difficulty: very fast breathing, struggling, noisy breathing, blue lips/face
- Severe bleeding that does not stop with firm pressure
- Seizure activity or repeated seizures
- Severe allergic reaction signs (especially breathing or swelling concerns)
- Serious head injury signs: worsening confusion, repeated vomiting, severe headache, abnormal behavior
- Severe burns, especially to face/airway, large areas, or chemical/electrical burns
- Suspected poisoning with concerning symptoms (sleepiness, breathing changes, seizures)
- Severe dehydration signs with lethargy or inability to keep fluids down
- Any situation where you feel the child is rapidly worsening
Decision rule: if you see a red flag, do not spend time searching online or debating. Call emergency services and begin supportive care while waiting.
Pathway 3: “Urgent today” vs “watchful waiting”
Not every problem is an emergency, but many require same-day evaluation. Use this pathway to decide between urgent care/doctor today and home observation.
Urgent today is appropriate when:
- The child is stable but symptoms are persistent, worsening, or unusual
- Pain is significant or increasing
- There is a concerning mechanism of injury (high fall, high-speed impact)
- The child has a chronic condition that increases risk (for example, significant asthma, immune compromise)
- You cannot reliably monitor the child (nighttime, no caregiver support, long travel)
Watchful waiting may be reasonable when:
- The child is alert, breathing comfortably, and improving
- Symptoms are mild and clearly linked to a minor event
- You can monitor closely and the child can drink fluids and rest
- You have clear criteria for when to escalate
Practical example: A child bumps their elbow and cries but then uses the arm normally within minutes. Watchful waiting with monitoring may be reasonable. If the child refuses to use the arm, pain increases, or swelling grows, that shifts to urgent evaluation.
Pathway 4: The “information handoff” pathway (what to report)
When you call emergency services, a school nurse, or a parent, clear information speeds care. Use a simple structure.
- Who: child’s age, known conditions, allergies if known
- What happened: mechanism (fall from height, hit by ball, found with open medication bottle)
- When: time of onset or injury
- What you see: breathing status, responsiveness, skin color, bleeding, pain location
- What you did: pressure applied, positioning, any medication given (name and dose if known)
- What changed: improving, stable, or worsening
Practical example script for a call: “This is a 6-year-old, no known allergies. Fell from monkey bars about 5 minutes ago. Awake, crying, breathing normally. No bleeding. Complains of wrist pain and won’t move it. We’ve kept the arm still and are monitoring. Pain is not improving.”
Step-by-step: a practical rapid assessment for infants and children
This is a general decision-support assessment to help you decide whether to escalate and what to do first. It is not a full medical exam.
Step 1: Scene and first impression (5–10 seconds)
- Is the area safe?
- Does the child look severely ill or injured?
- Are they interacting normally for age?
- Are they breathing comfortably?
- Is there obvious severe bleeding?
If the first impression is concerning, move immediately to emergency activation and supportive actions.
Step 2: Responsiveness and interaction
- Speak to the child, use their name if known.
- For infants, observe alertness: do they track you, respond to voice, cry normally?
- Note unusual sleepiness, confusion, or inability to be consoled.
Practical example: A toddler who is normally active sits quietly and does not respond to a favorite toy. That change in interaction is a warning sign even if there is no visible injury.
Step 3: Breathing check (look, listen, feel)
- Look for chest movement and effort (retractions, flaring, posture).
- Listen for noisy breathing, wheeze, or silence when you expect sound.
- Check if they can speak in full sentences (older child) or cry strongly (infant/toddler).
If breathing is difficult, prioritize emergency help and positioning for easier breathing. Avoid forcing the child to lie flat if that worsens breathing.
Step 4: Circulation and bleeding
- Scan quickly for severe bleeding and control it with firm pressure.
- Observe skin color and sweating.
- Check for signs of poor circulation: pale, cool, clammy, weak responsiveness.
In children, shock can develop even when bleeding is not obvious. If the child looks pale and weak after an injury, treat it seriously and seek urgent help.
Step 5: Focused check based on the story
Use the mechanism and symptoms to guide a focused check rather than a head-to-toe search that delays action.
- Fall or impact: check head/neck symptoms, limb function, pain location.
- Possible ingestion: check mental status, breathing, vomiting, and gather substance information.
- Fever/unwellness: check hydration, breathing effort, rash, and alertness.
Practical example: After a bicycle crash, you focus on head symptoms, breathing, and limb movement rather than spending time on minor scrapes first.
Step 6: Decide and act
Choose one of three actions:
- Emergency response: red flags present or rapid worsening.
- Urgent evaluation today: stable but concerning symptoms, significant pain, or inability to monitor.
- Home care with monitoring: mild symptoms, improving, reliable observation possible.
Communication and teamwork in home and school settings
Assign roles to reduce errors
In group settings, errors happen when everyone assumes someone else is calling for help or watching the child. Assign roles explicitly.
- Caller: contacts emergency services/parent and stays on the line.
- First aider: stays with the child and performs immediate care.
- Runner: retrieves first aid kit, AED if available, medication authorization forms if relevant.
- Crowd control: keeps other children back and clears space.
Use child-centered language
Explain what you are doing in simple terms. Offer choices when possible to increase cooperation.
- “I’m going to put my hand here to stop the bleeding.”
- “Do you want to sit on the bench or on the grass while we wait?”
- “Show me where it hurts with one finger.”
Managing caregivers’ emotions
In schools and public places, a distressed parent can unintentionally interfere. Give them a task and clear updates.
- “Please stand right here so your child can see you.”
- “I need you to tell me any allergies or medical conditions.”
- “We are watching breathing and alertness; if anything changes we will call again immediately.”
Decision-making under uncertainty: practical rules that prevent harm
Rule 1: If you are debating whether it is serious, treat it as potentially serious
Uncertainty is common. If you cannot confidently say the child is stable and improving, choose the safer path: escalate or seek same-day evaluation.
Rule 2: Worsening beats “normal vitals”
You may not have tools to measure vital signs. Even if the child looks “okay,” a trend toward worsening behavior, breathing effort, or color is a strong reason to escalate.
Rule 3: Mechanism matters
A child may look fine immediately after a significant event. High-energy mechanisms (high falls, vehicle impacts) increase risk of hidden injury. Use a lower threshold for urgent evaluation even if symptoms are mild at first.
Rule 4: When in doubt, do less but do it well
High-quality first aid is often simple: keep the child safe, still when needed, warm, reassured, and monitored; control severe bleeding; call for help early. Avoid unnecessary movement and unnecessary oral intake if there is any chance of serious injury or reduced alertness.
Mini-scenarios: applying the pathways
Scenario A: “Not acting right” after a minor bump
A 4-year-old bumps their head on a table edge. There is a small bruise, no bleeding. Ten minutes later, they are unusually quiet and want to lie down.
- Stop–Check: safe scene, child responsive but subdued, breathing normal, no severe bleeding.
- Red flags? Behavior change is concerning, especially if worsening.
- Act: keep them resting, monitor alertness and vomiting, and seek urgent medical advice/evaluation if the behavior change persists or worsens.
- Recheck: if they become difficult to wake, vomit repeatedly, or develop worsening headache/confusion, escalate to emergency response.
Scenario B: Playground injury with obvious deformity
A child falls and the forearm looks bent. They are crying and guarding the arm.
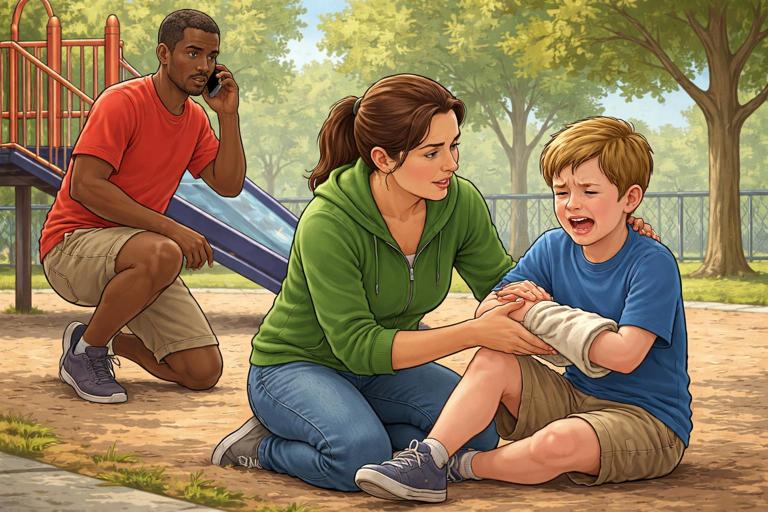
- Stop–Check: ensure area is safe; child is alert and breathing normally.
- Act: keep the limb still in the position found, support it, control any bleeding, and arrange urgent evaluation. Do not attempt to straighten the limb.
- Recheck: monitor for increasing pain, pale/cool hand, or numbness, which increases urgency.
Scenario C: Possible ingestion at home
You find an open bottle of medication near a toddler. The child seems normal.
- Stop–Check: remove remaining pills from reach; do not induce vomiting or give food/drink unless advised by professionals.
- Act: call poison control/emergency services per local guidance with the medication name, strength, and estimated amount missing.
- Recheck: monitor for sleepiness, vomiting, breathing changes, or unusual behavior while awaiting instructions.
Scenario D: Breathing concern during sports
An older child is short of breath after running and cannot speak full sentences comfortably.
- Stop–Check: sit them upright, calm coaching, assess breathing effort and color.
- Red flags? Trouble speaking, visible struggle, or bluish color indicates emergency.
- Act: activate emergency response if severe; otherwise seek urgent evaluation and monitor closely for worsening.
Practical tools: simple scripts and checklists you can keep accessible
Emergency call script (fill in blanks)
We have a child emergency at: [address/location details]. The child is: [age]. They are: [awake/unresponsive]. Breathing is: [normal/difficult/not breathing]. There is: [severe bleeding/no severe bleeding]. The problem started: [time]. We are doing: [pressure/monitoring/positioning]. Please send help.Escalation checklist for caregivers
- I am worried about breathing, alertness, or color.
- Symptoms are worsening or not improving as expected.
- The injury mechanism was significant.
- I cannot monitor reliably for the next several hours.
- The child has higher risk due to medical history.
If any item is true, choose a higher level of care rather than waiting.