Why Head Injuries Matter in Home and School Settings
Head injuries are common in infants and children because their heads are proportionally larger, their balance and coordination are still developing, and they spend a lot of time climbing, running, and playing. Most bumps to the head are minor and heal without problems, but some can cause a concussion or a more serious brain injury. The challenge in homes and schools is that a child may look “mostly fine” right after the incident and then develop concerning symptoms later. This chapter focuses on recognizing concussion warning signs, identifying red flags that suggest a more serious injury, and providing practical, step-by-step care and monitoring in everyday settings.
A “head injury” can involve the scalp, skull, or brain. A concussion is a type of mild traumatic brain injury caused by a blow to the head, face, neck, or body that transmits force to the brain. Concussions can happen without loss of consciousness. They can also occur from a fall where the head does not obviously strike something, especially if the body stops suddenly (for example, a collision during sports or a sudden stop on a playground slide).
Common Causes at Home and at School

Home
- Falls from beds, couches, changing tables, stairs, or high chairs
- Slipping in bathrooms or on wet floors
- Collisions with furniture edges, doors, or countertops
- Being struck by falling objects (books, decor, tools)
- Bike/scooter falls in driveways and sidewalks
School and childcare
- Playground falls (monkey bars, swings, climbing structures)
- Running collisions in hallways or on the field
- Sports impacts (balls, elbows, head-to-head contact)
- Falls from chairs or during gym activities
- Rough play or accidental pushes
Mechanism matters: higher-force events (fall from significant height, high-speed sports collision, being hit by a moving object) increase concern even if symptoms seem mild at first.
What Happens in a Concussion (Clear Concept Explanation)
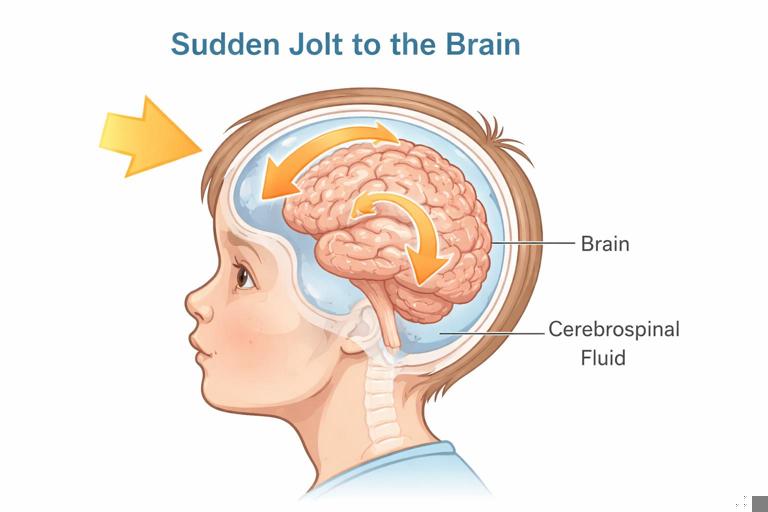
The brain sits in fluid inside the skull. A sudden jolt can cause the brain to move and twist, stretching nerve cells and changing how the brain uses energy. This can lead to symptoms such as headache, dizziness, confusion, sensitivity to light/noise, and changes in mood or sleep. These symptoms may appear immediately or develop over minutes to hours. In children, symptoms can be subtle and may look like behavior problems, “not listening,” or unusual tiredness.
Concussion symptoms usually improve with time and appropriate management, but returning to full activity too soon can worsen symptoms and prolong recovery. A second head impact before recovery can be dangerous. In home and school settings, the practical goal is to recognize possible concussion, protect the child from further injury, and ensure appropriate medical evaluation and follow-up.
- Listen to the audio with the screen off.
- Earn a certificate upon completion.
- Over 5000 courses for you to explore!
Download the app
First Priorities After a Head Impact: Step-by-Step
Step 1: Stop the activity and stabilize the situation
Immediately stop play, sports, or any activity. Keep the child still and calm. If the incident involved a fall from height, a high-speed collision, or the child complains of neck pain, avoid moving them unnecessarily and keep the head and neck aligned.
Step 2: Quick check for immediate danger signs
Look for signs that suggest a serious head or neck injury. If any are present, treat it as an emergency and seek urgent medical help. Examples include: the child is difficult to wake, has repeated vomiting, has worsening headache, has a seizure, has weakness or numbness, has slurred speech, has unequal pupils, has blood or clear fluid from the nose/ears, or has significant confusion that is not improving.
Also treat as urgent if there is a large scalp wound with uncontrolled bleeding, a deep cut with visible tissue, or a suspected skull fracture (for example, a soft “boggy” swelling in an infant, a dented area, or bruising behind the ears or around the eyes not explained by a direct hit).
Step 3: If no immediate danger signs, assess for concussion symptoms
Ask simple questions and observe. In a school setting, use calm, concrete prompts. In younger children, rely more on behavior and caregiver reports. Concussion is suspected when symptoms occur after a head impact or body jolt, even if the child did not lose consciousness.
Step 4: Protect from a second injury
Do not allow the child to return to sports, recess, climbing, biking, or rough play the same day if concussion is suspected. Keep them supervised. A second hit while symptomatic increases risk.
Step 5: Inform caregivers and document key details
Record the time and location of the injury, what happened (mechanism), whether there was any loss of consciousness, immediate symptoms, and any changes over time. At school, follow your incident reporting process. At home, write notes to share with a clinician if needed.
Concussion Warning Signs: What to Look For
Concussion symptoms fall into several categories. A child may have only a few, and they may fluctuate.
Physical symptoms
- Headache or “pressure” in the head
- Dizziness, balance problems, unsteady walking
- Nausea or vomiting (vomiting more than once is more concerning)
- Blurred or double vision
- Sensitivity to light or noise
- Feeling tired, low energy
- Ringing in the ears
Thinking and learning symptoms
- Confusion, seeming “foggy” or slowed down
- Difficulty concentrating or remembering
- Answering questions slowly
- Not following instructions that are normally easy
Emotional and behavior symptoms
- Irritability, unusual anger, tearfulness
- Anxiety, nervousness
- Personality changes that are out of character
Sleep-related symptoms
- Drowsiness, sleeping more than usual
- Trouble falling asleep or staying asleep
Infants and toddlers: special clues
Very young children cannot describe headache or dizziness. Watch for:
- Persistent crying or inability to be consoled
- Refusing to eat or nurse, repeated spit-up/vomiting beyond usual
- Changes in play interest, not engaging with caregivers
- Unsteady sitting/standing beyond their baseline
- Sleepiness at unusual times or difficulty waking
- Staring spells or “not acting right” as reported by a caregiver
Red Flags That Suggest a More Serious Brain Injury

Some symptoms require urgent medical evaluation because they may indicate bleeding in or around the brain or significant swelling. Seek urgent help if any of the following occur after a head injury:
- Loss of consciousness (especially prolonged) or the child cannot be awakened normally
- Repeated vomiting or vomiting that starts/worsens hours later
- Worsening headache, especially if severe or not relieved by usual measures
- Seizure activity
- Weakness, numbness, clumsiness on one side, or trouble walking
- Slurred speech, confusion that is worsening, or unusual behavior that is escalating
- Unequal pupils, new vision changes, or persistent double vision
- Blood or clear fluid leaking from the nose or ears
- Large swelling on the scalp in an infant, a dented area, or suspected skull fracture
- Neck pain with limited movement, or tingling in arms/legs after a fall
- Any concern for abuse or an injury story that does not match the child’s developmental abilities
In schools, treat these as immediate escalation events. In homes, do not “wait and see” if red flags are present.
Scalp Bumps, Cuts, and Nosebleeds: Practical Care Without Over- or Under-Reacting
Scalp bumps (“goose eggs”)
The scalp has many blood vessels, so bumps can look dramatic. A large bump does not automatically mean a serious brain injury, but it does mean you should monitor carefully for concussion symptoms and red flags.
- Apply a cold pack wrapped in cloth for 10–15 minutes at a time to reduce pain and swelling.
- Keep the child calm and seated; avoid immediate return to active play.
- Re-check symptoms over the next several hours.
Scalp cuts
Scalp cuts can bleed heavily. Control bleeding with firm, steady pressure using clean gauze or cloth. If the cut is gaping, bleeding does not stop with pressure, or you can see deeper tissue, the child likely needs medical evaluation for closure. If there is a possibility of a skull fracture (dented area, severe pain, high-force mechanism), avoid pressing directly on a suspected depressed area and seek urgent care.
Nosebleed after a facial impact
A nosebleed can occur with facial bumps. Manage the nosebleed with forward-leaning posture and gentle pinching of the soft part of the nose. If the nose looks crooked, there is significant facial swelling, or there are concussion symptoms, arrange medical evaluation. If there is clear fluid from the nose after head trauma, treat as a red flag.
Observation and Monitoring: A Practical Home/School Plan
How long to monitor
Most concerning symptoms show up within the first 24 hours, but some appear later. Plan for close observation for the rest of the day and continued awareness over the next 1–2 days.
What “close observation” means
- Stay within sight and hearing of the child for several hours after the injury.
- Re-check symptoms every 30–60 minutes early on: headache, nausea, dizziness, confusion, behavior changes.
- Limit activities that increase risk of another fall or collision.
- Ensure the child can be awakened and interacts normally for them.
Sleep after a head injury
It is common for children to feel tired. Sleep is not automatically dangerous. The practical concern is whether the child can be awakened and is behaving appropriately when awake. If a clinician has not advised otherwise, allow sleep but check periodically to ensure normal breathing and that the child can be roused and responds in a typical way. If the child is unusually difficult to wake or becomes increasingly confused, treat as urgent.
What to write down (helps clinicians and schools)
- Time of injury and time symptoms began
- Mechanism (fall height, collision, object hit, speed)
- Immediate signs: dazed, confused, cried right away, any loss of consciousness
- Symptoms over time: headache rating, vomiting episodes, behavior changes
- Any medications given and when
Return-to-Learn and Return-to-Play: Practical School and Home Adjustments
After a suspected or diagnosed concussion, the child’s brain may be more sensitive to exertion. Symptoms often worsen with physical activity and also with cognitive load (reading, screens, tests). The goal is a gradual return to normal activities without triggering symptom spikes.
Return-to-learn supports (school-focused)
Even if a child looks fine, they may struggle with concentration, noise, and bright lights. Practical supports include:
- Shortened school day or rest breaks in a quiet area
- Reduced homework load for a few days
- Extra time for assignments and tests
- Postponing high-stakes testing until symptoms improve
- Limiting screen time at school if it triggers headache
- Preferential seating away from bright windows or noisy areas
Example: A 10-year-old hit their head during recess and later reports headache and “feeling weird.” The next day, the teacher notices slower work and irritability during reading. Provide a quiet break, reduce reading time, and notify caregivers that symptoms are persisting and may require medical follow-up.
Return-to-play precautions (home and school sports)
If concussion is suspected, no same-day return to sports or vigorous play. Return to sports should be gradual and typically guided by a healthcare professional or school athletic policy. A practical rule for caregivers and staff is: if symptoms return during activity, stop and step back to the previous level of activity after rest.
Example: A middle-school student feels fine at rest but develops headache during light jogging at practice. They should stop immediately, rest, and report symptoms; they should not “push through.”
Special Situations and Higher-Risk Scenarios
Infants: falls and “short drops”
Infants may fall from beds or changing surfaces. Even if the fall seems short, infants can have significant injury. Watch closely for changes in feeding, alertness, vomiting, and unusual swelling on the scalp. A large, soft swelling or a child who is not acting normally warrants prompt evaluation.
Children with bleeding disorders or on blood-thinning medication
These children have a higher risk of bleeding after head trauma. Any significant head impact should be discussed promptly with a clinician, even if symptoms are mild.
Children with previous concussions
Prior concussion can increase vulnerability and may prolong recovery. Take symptoms seriously and avoid rapid return to full activity.
Suspected abuse (non-accidental trauma)
If the story does not match the injury, if there are multiple injuries, or if there is concern about shaking or intentional harm, treat it as a medical emergency and follow your local safeguarding and reporting procedures. Do not confront; focus on the child’s safety and appropriate escalation.
What to Say and Do in the Moment: Practical Scripts
For a child who is anxious after a head bump
Use calm, simple reassurance and clear instructions: “You had a hard bump. We’re going to sit together and rest. I’m going to ask you a few questions and watch you closely. If anything feels worse—like your head hurts more or you feel sick—tell me right away.”
For notifying caregivers (school or childcare)
Share objective details and current symptoms: “At 12:20, your child fell from the climbing structure and hit the side of their head. They did not lose consciousness. They reported headache and seemed a bit slowed answering questions. They are resting and not returning to play today. Please monitor closely at home and seek medical care urgently if vomiting, worsening headache, confusion, or unusual sleepiness occurs.”
Common Mistakes to Avoid
- Assuming “no loss of consciousness” means “no concussion.”
- Allowing same-day return to sports or rough play after a suspected concussion.
- Ignoring subtle symptoms like irritability, concentration problems, or unusual fatigue.
- Focusing only on the size of the bump rather than the child’s behavior and symptoms.
- Failing to document the mechanism and symptom timeline, which are crucial for medical decisions.
Quick Reference: Concussion Symptom Check (Use in Home/School Notes)
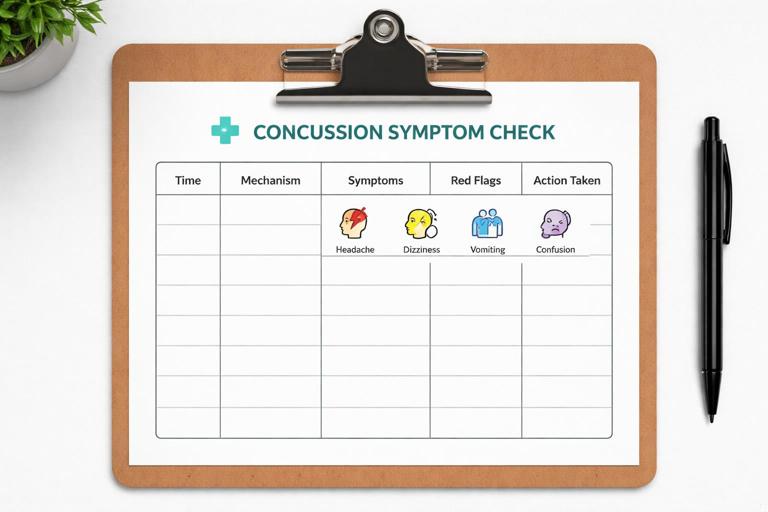
After head impact/body jolt, check and record: Time of injury: ____ Mechanism: ____ Witnessed? Y/N Loss of consciousness? Y/N Neck pain? Y/N Symptoms now (circle): Headache Dizziness Nausea Vomiting Balance issues Vision changes Light/noise sensitivity Confusion Slow responses Memory problems Irritability Sleepiness Other: ____ Red flags present? (repeated vomiting, worsening headache, seizure, weakness, unequal pupils, blood/clear fluid from nose/ears, hard to wake): Y/N Action taken: Rest/supervision, removed from play, caregiver notified, medical evaluation arranged.