What “Drowning” and “Near-Drowning” Mean
Drowning is a process in which breathing is impaired because the airway is under water or another liquid. It can happen in a pool, bathtub, lake, bucket, toilet, hot tub, or even during play with hoses and water tables. “Near-drowning” is an older term often used to describe a child who survives the event initially. In real life, the same emergency can look mild at first and then worsen later, so the key idea is this: any episode where a child was submerged, struggled to breathe, inhaled water, or had a coughing/choking spell after being in water should be treated as potentially serious.
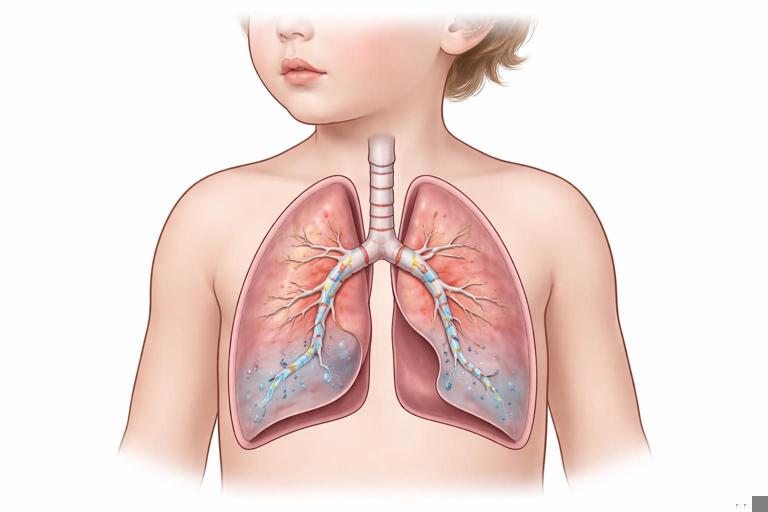
Water in the airway can trigger laryngospasm (the vocal cords clamp shut), swelling, and irritation. Even small amounts of aspirated water can inflame the lungs and interfere with oxygen exchange over the next several hours. Cold water can also contribute to hypothermia, which affects breathing, heart rhythm, and alertness. Because children have smaller airways and less oxygen reserve than adults, they can deteriorate quickly.
Rescue Priorities: The Order That Keeps Rescuers and Children Alive
1) Rescuer safety comes first
Many drownings involve a second victim: a parent, sibling, or bystander who enters the water and is pulled under. A panicking child may climb onto you, pushing you down. Your first job is to avoid becoming another person who needs rescue.
- Do not jump in unless you are trained and conditions are safe.
- Use a “reach or throw” approach when possible: reach with a pole, towel, branch, pool skimmer, or throw a flotation device.
- If you must enter shallow water, keep your feet on the bottom and extend a tool rather than your body.
- If you are in a boat or on a dock, lie down to lower your center of gravity before reaching out.
2) Get the child out of the water as quickly as possible
Once the child is within reach, bring them to a stable surface. If you are alone, prioritize removing them from the water over gathering belongings or searching for towels. If others are present, assign tasks: one person retrieves flotation or a phone, another clears space for care.
3) Check breathing immediately and act
Drowning is primarily a breathing problem. The most important early actions are to restore breathing and oxygenation. If the child is not breathing normally, begin resuscitation steps right away. If the child is breathing, focus on airway positioning, warmth, and monitoring.
- Listen to the audio with the screen off.
- Earn a certificate upon completion.
- Over 5000 courses for you to explore!
Download the app
What to Do in the First Minutes After Rescue (Practical Steps)
If the child is unresponsive and not breathing normally
Start resuscitation immediately. In drowning, early ventilation is especially important because lack of oxygen is the main issue. If you are trained, provide rescue breaths and follow your local pediatric resuscitation protocol. If an AED is available, have someone bring it and use it as soon as possible. Continue until the child breathes normally, professional help takes over, or you are physically unable to continue.
Practical points specific to drowning scenes:
- Do not waste time trying to “drain” water from the lungs by holding the child upside down or pressing on the abdomen. This delays ventilation and can cause vomiting and aspiration.
- Expect vomiting. Turn the child’s head to the side if possible while maintaining an open airway. Clear the mouth only if you can see material that can be removed easily.
- Wet clothing can worsen cooling. Once resuscitation is underway and help is coming, remove wet clothing if it can be done quickly without interrupting critical care, and cover with dry towels/blankets.
If the child is unresponsive but breathing
Place the child on their side in a recovery position to keep the airway open and reduce aspiration risk if vomiting occurs. Keep the head and neck aligned; avoid excessive neck movement. Continue to watch breathing closely. A child can shift from “breathing” to “not breathing” in seconds if the airway closes or swelling increases.

If the child is awake, crying, or coughing
This can still be serious. Coughing is a protective reflex, but persistent coughing after submersion suggests water irritation or aspiration. Your priorities are:
- Keep the child calm and still; crying and agitation increase oxygen demand.
- Encourage slow, steady breathing. Do not force deep breaths.
- Keep them warm: remove wet clothing and wrap in dry layers.
- Do not give food or drink right away. Swallowing may trigger coughing or vomiting.
- Observe continuously for any change in breathing effort, color, or alertness.
When to Seek Emergency Evaluation After a Water Incident
Any of the following after submersion should be treated as a medical emergency and evaluated urgently, even if the child seems “mostly fine”:
- Any period of unconsciousness, even brief
- Any need for resuscitation or assisted breathing
- Persistent cough, wheeze, or noisy breathing
- Fast breathing, labored breathing, chest retractions, nasal flaring, or grunting
- Blue/gray lips or face, or unusual paleness
- Vomiting more than once, especially with ongoing cough
- Sleepiness, confusion, unusual behavior, headache, or difficulty walking/talking
- Low energy, weakness, or the child “just isn’t themselves”
- Cold exposure with shivering that won’t stop, or a child who is cold and not shivering
- Submersion in very cold water, unknown duration, or contaminated water (lake/river/floodwater)
Even if symptoms are mild, many clinicians recommend observation for a period of time because lung irritation can evolve. If you are unsure, err on the side of medical assessment.
Understanding Delayed Breathing Problems After Drowning
Families sometimes hear alarming phrases like “secondary drowning” or “dry drowning.” These terms are not consistently used in medicine, but they point to a real concern: breathing can worsen after the event due to airway spasm, inflammation, and fluid shifts in the lungs. The practical takeaway is not the label—it is the monitoring.
After aspiration, the lungs may develop irritation that looks like asthma or pneumonia: coughing, wheezing, rapid breathing, and low oxygen. Symptoms can appear soon after the incident or develop gradually over several hours. A child who is exhausted after a scare may also fall asleep; it can be hard to tell normal fatigue from early oxygen problems unless you know what to watch for.
Post-Event Monitoring at Home: A Structured Approach
Only monitor at home if the child had a minor incident (for example, brief splash/submersion with immediate recovery), is now completely normal, and you have access to urgent care if symptoms appear. If there was any doubt about breathing, any altered alertness, or any need for resuscitation, seek medical evaluation rather than relying on home monitoring.
What to watch for (the “breathing, brain, and body” check)
- Breathing: cough that persists or worsens; breathing faster than usual; working harder to breathe (ribs pulling in, belly breathing, flaring nostrils); noisy breathing; pauses in breathing; complaints of chest tightness; inability to speak in full sentences (older children).
- Brain/behavior: unusual sleepiness, hard to wake, confusion, irritability out of proportion, dizziness, fainting, headache, or “acting drunk.”
- Body signs: blue/gray lips, cool clammy skin, repeated vomiting, fever later in the day (can occur with aspiration-related inflammation), or worsening fatigue.
How to monitor practically (step-by-step)
Step 1: Set up a calm observation space. Keep the child nearby, warm, and resting. Avoid vigorous play for the rest of the day because exertion can unmask breathing difficulty.
Step 2: Check breathing effort regularly. Look at the chest and belly. Is breathing easy and quiet, or is it fast and strained? Listen for wheeze, gurgling, or persistent throat clearing.
Step 3: Check color and circulation. Lips should be pink (or normal baseline color). Hands and feet may be cool after water exposure, but the face and lips should not look dusky or gray.
Step 4: Check alertness. The child should be oriented for their age: making eye contact, responding normally, and waking easily if they nap. If they sleep, you should be able to rouse them and get a normal response.
Step 5: Track symptoms over time. Note the time of the incident and any symptoms. Worsening cough, increasing breathing rate, or increasing sleepiness are red flags.
Step 6: Know your escalation triggers. If any breathing difficulty appears, if coughing becomes persistent, if vomiting repeats, or if behavior changes, seek urgent medical care immediately.
Common caregiver questions during monitoring
“Should I keep them awake?” You do not need to force a child to stay awake if they are otherwise normal, but you should be able to wake them easily and they should act normally when awake. If they are difficult to rouse or seem confused, that is not normal fatigue.
“Can I give them something to drink?” If they are fully alert and not coughing, small sips may be reasonable. Avoid large volumes right away. If coughing or nausea is present, wait and seek medical advice.
“What about a pulse oximeter?” Home pulse oximeters can be helpful but are not foolproof, especially with cold fingers, movement, or poor fit. Do not let a “normal number” override visible breathing effort or concerning behavior.
Special Situations
Bathtub and infant incidents
Infants can drown in very small amounts of water and may not splash or cry. If an infant was found face-down, silent, or limp—even briefly—treat it as a high-risk event. Infants also cool quickly, and hypothermia can make them appear sleepy or weak. Seek emergency evaluation after any significant bathtub submersion or any episode with coughing, color change, or altered responsiveness.
Cold water submersion
Cold water can trigger a gasp reflex and rapid breathing, increasing the chance of inhaling water. It also causes rapid heat loss. After rescue:
- Remove wet clothing and insulate with dry layers.
- Handle gently; severe hypothermia can make the heart irritable.
- Do not apply intense direct heat (like very hot baths) to a cold child; use gradual warming with blankets and body heat while awaiting medical guidance.
Contaminated water (lakes, rivers, floodwater)
These exposures increase the risk of lung infection and chemical irritation. Even if the child looks well, clinicians may recommend evaluation depending on symptoms and exposure details. Watch closely for fever, worsening cough, chest pain, or breathing difficulty later.
Diving injuries and water slides
If the incident involved diving, collision, or a fall into shallow water, consider possible neck or spine injury. In that case, keep the head and neck as still as possible while getting help. Do not attempt complicated maneuvers in the water; prioritize safe rescue and professional assistance.
Vomiting and Airway Protection After Drowning
Vomiting is common after submersion due to swallowed water, stress, and resuscitation efforts. The danger is aspiration (vomit entering the lungs). Practical steps:
- Keep the child on their side if they are drowsy or nauseated.
- Have a towel or cloth ready; clear the mouth only if you can see material.
- After vomiting, reassess breathing: listen for new wheeze, gurgling, or increased work of breathing.
- If vomiting repeats or the child cannot keep their airway clear, seek urgent care.
What to Document for Medical Teams (and for Your Own Clarity)
In a stressful event, details blur. Writing down key facts helps clinicians judge risk and decide on observation or tests. Useful details include:
- Where it happened (pool, bathtub, lake), and whether water was cold or contaminated
- Estimated submersion time (even a guess)
- What the child looked like when found (coughing, silent, limp, blue lips)
- Whether the child cried immediately after rescue or was initially quiet
- Any resuscitation performed and for how long
- Symptoms since the event: cough, vomiting, breathing changes, sleepiness
- Any medical history that affects breathing (asthma, prematurity, heart conditions)
Practical Scenarios (How Priorities Change)

Scenario 1: Toddler pulled from a pool, coughing but awake
The child is crying and coughing, then settles. You dry and warm them, keep them close, and watch breathing. If coughing persists beyond a short period, if breathing becomes fast or labored, or if the child becomes unusually sleepy, you seek urgent evaluation. You avoid giving snacks immediately and keep activity low.
Scenario 2: Child found face-down in a bathtub, briefly unresponsive
This is high risk even if the child “comes around.” Emergency evaluation is warranted. While waiting, keep the airway open, place on the side if vomiting risk is present, keep warm, and monitor breathing continuously.
Scenario 3: Teen pulled from a lake after struggling, now shivering and exhausted
Warmth and breathing assessment are both priorities. Remove wet clothing, wrap in dry blankets, and monitor for worsening breathing or confusion. Cold exposure can mask symptoms; if there was significant submersion or inhalation of water, medical evaluation is appropriate.
Prevention Notes Tied to Rescue Readiness (Without Repeating General Safety Chapters)
Because drowning is fast and silent, preparedness matters. Practical readiness steps include:
- At gatherings near water, designate an adult “water watcher” for short shifts who does nothing else (no phone, no cooking).
- Keep rescue tools visible: a reaching pole, life ring, or throw rope near pools.
- Teach children to float and to reach/throw rather than jump in to help a friend.
- After any water incident, treat it as a medical event, not just a scare—monitor and escalate based on symptoms.