What Allergic Reactions Are (and Why They Can Escalate)
An allergic reaction happens when the immune system treats a normally harmless substance as a threat and releases chemicals (including histamine) that cause symptoms in the skin, nose, lungs, gut, or whole body. In infants and children, reactions can be mild and limited to one area (for example, a few hives around the mouth after a new food) or can rapidly involve multiple body systems. The most dangerous form is anaphylaxis: a severe, fast-moving allergic reaction that can affect breathing and circulation. Anaphylaxis is time-sensitive because swelling, airway narrowing, and a sudden drop in blood pressure can progress quickly.
Not every rash is an allergy, and not every allergy becomes anaphylaxis. The key for caregivers is to recognize patterns that suggest an allergic cause, identify when the reaction is becoming systemic, and act decisively with the correct medication and monitoring.
Common triggers in home, school, and everyday settings

- Foods: peanuts, tree nuts, milk, egg, wheat, soy, fish, shellfish, sesame. Cross-contact (shared utensils, surfaces, fryer oil) is a frequent cause outside the home.
- Stinging insects: bees, wasps, hornets, fire ants.
- Medications: antibiotics (especially penicillins/cephalosporins), NSAIDs, some vaccines (rarely), and others.
- Latex: balloons, gloves, some medical devices.
- Environmental allergens: pollen, dust mites, animal dander (more often cause nasal/eye symptoms or asthma flares than anaphylaxis).
- Exercise or heat: can trigger or worsen reactions in some children, sometimes in combination with food (food-dependent exercise-induced anaphylaxis).
Recognizing Mild/Moderate Allergic Reactions vs. Anaphylaxis
Allergic reactions often start with skin symptoms, but anaphylaxis can begin without hives. Use a “systems” approach: skin, breathing, circulation, and gut/neurologic symptoms. The more systems involved, the higher the risk.
Typical mild to moderate allergic reaction signs
- Skin: localized hives, itching, mild swelling (for example, a few hives on the face), redness.
- Nose/eyes: sneezing, runny nose, itchy watery eyes.
- Mouth: mild lip itch or tingling without swelling or breathing issues.
- Gut: mild nausea or a single episode of vomiting without other symptoms (can still be early anaphylaxis if linked to an allergen exposure—watch closely).
Signs that suggest anaphylaxis (treat as an emergency)
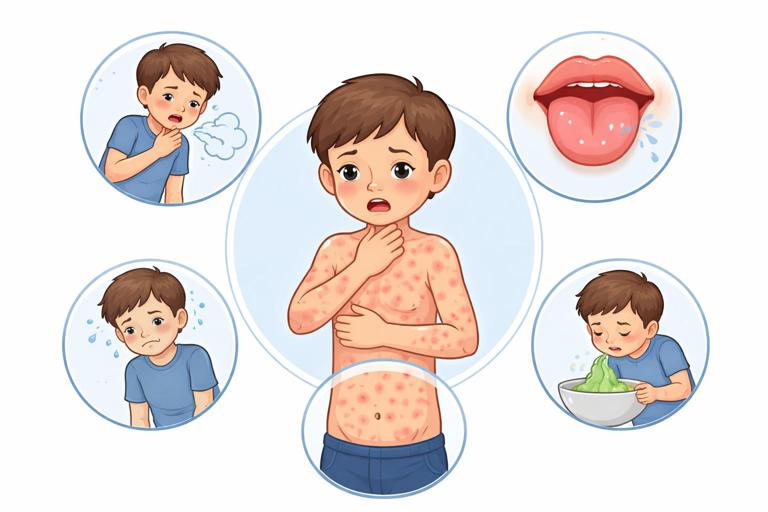
- Breathing/airway: wheeze, repetitive cough, hoarse voice, trouble speaking/crying normally, noisy breathing/stridor, throat tightness, swelling of tongue, drooling due to difficulty swallowing.
- Circulation: pale or gray color, faintness, collapse, weak pulse, confusion, unusually sleepy or “not acting right,” low blood pressure (hard to measure at home, but look for dizziness, limpness, poor responsiveness).
- Multiple body systems: hives plus vomiting; hives plus wheeze; swelling plus cough; or any rapid progression after exposure.
- Severe gut symptoms: repeated vomiting, severe crampy abdominal pain, especially with other symptoms.
- Infants-specific clues: sudden persistent crying, sudden lethargy, floppy tone, vomiting after exposure, facial swelling, widespread hives, or a sudden change in breathing pattern. Infants cannot describe throat tightness—watch for voice/cry changes and increased work of breathing.
Important: If a child has a known severe allergy and has been exposed to their trigger, treat early if symptoms begin. Waiting “to see if it gets worse” is a common reason for delayed epinephrine.
Core Principle: Epinephrine First for Anaphylaxis
Epinephrine (adrenaline) is the first-line treatment for anaphylaxis. It works quickly to open airways, reduce swelling, and support blood pressure. Antihistamines can help itching and hives but do not treat airway swelling or shock. Inhalers may help wheeze in a child with asthma, but they do not replace epinephrine in anaphylaxis.
- Listen to the audio with the screen off.
- Earn a certificate upon completion.
- Over 5000 courses for you to explore!
Download the app
Caregivers sometimes hesitate because they fear “overreacting.” In practice, the risk of delaying epinephrine is greater than the risk of giving it when it turns out not to be anaphylaxis. When in doubt and symptoms suggest anaphylaxis, use the auto-injector.
What about antihistamines and steroids?
- Antihistamines (e.g., cetirizine, loratadine, diphenhydramine): can reduce hives/itching. They do not prevent airway compromise or shock. Use only if the child can swallow safely and is not having breathing or severe symptoms.
- Oral steroids: sometimes prescribed after a reaction, but they are slow-acting and not a rescue medication.
Step-by-Step Action Plan for Suspected Anaphylaxis
Use these steps when a child has symptoms consistent with anaphylaxis or a rapidly worsening allergic reaction. Adapt them to your setting (home, playground, classroom, restaurant).
Step 1: Stop exposure and assess quickly
- Remove the trigger if possible (stop eating the food, move away from insects, remove latex source).
- If there is a stinger visible after a bee sting, remove it promptly by scraping with a card or fingernail. Do not spend extra time searching if it is not obvious.
- Look for breathing difficulty, voice changes, widespread hives, swelling, vomiting, or collapse.
Step 2: Give epinephrine immediately if criteria are met

If the child has breathing symptoms, circulation symptoms, or multiple-system involvement after exposure, give epinephrine right away. If the child has a known severe allergy and has been exposed and is developing symptoms, treat early.
Step 3: Correct position and supportive care while monitoring
- If dizzy, faint, or very weak: lay the child flat on their back if they can breathe comfortably. Elevate legs if tolerated.
- If vomiting or very nauseated: place on their side to protect the airway.
- If breathing is difficult: allow a position of comfort (often sitting up slightly). Avoid sudden standing or walking.
- Keep warm with a blanket or jacket.
- Do not give food or drink during severe symptoms.
Step 4: Arrange urgent medical evaluation and continued observation
Anaphylaxis requires medical evaluation even if the child improves after epinephrine, because symptoms can return (biphasic reaction) or worsen again as the medication wears off. Plan for transport to emergency care and continued monitoring.
Step 5: Be ready to give a second dose
If symptoms are not improving or are returning, a second epinephrine dose may be needed. Many action plans allow repeating epinephrine after about 5–15 minutes if severe symptoms persist. Follow the child’s prescribed plan and local emergency guidance.
How to Use an Epinephrine Auto-Injector (Practical Technique)
Different brands have slightly different instructions, but the core technique is similar. Always read the device label and the child’s action plan in advance. Practice with a trainer device if available.
Step-by-step technique (general)
- 1) Retrieve the auto-injector quickly. Check that it is the correct device for the child and not expired if time allows (do not delay treatment to check).
- 2) Remove safety cap(s). Hold the device in your fist with the needle end pointing down (avoid placing thumb over either end).
- 3) Place against the outer mid-thigh. The outer thigh is the preferred site. It can be given through clothing if needed (avoid thick seams or items in pockets).
- 4) Press firmly until it activates. You may hear or feel a click. Keep it in place for the time specified by the device instructions (often a few seconds).
- 5) Remove and massage the area briefly if recommended by the device instructions.
- 6) Note the time given. This helps medical staff and helps you decide about a second dose if symptoms persist.
- 7) Secure the used device. Give it to medical personnel for disposal and confirmation of dose/time.
Preventing injection injuries in young children
- Young children may kick or pull away. If possible, have another adult stabilize the child’s leg.
- For infants/toddlers, place the child on your lap or on the ground and hold the thigh firmly to prevent sudden movement.
- Do not inject into buttock, hands, feet, or other areas.
Common caregiver mistakes to avoid
- Waiting for hives: anaphylaxis can occur without skin symptoms.
- Using antihistamine first: it can delay epinephrine and does not treat airway/circulation problems.
- Standing the child up: sudden standing can worsen low blood pressure.
- Not carrying two doses: some reactions require a second dose before help arrives.
- Not calling for medical evaluation after improvement: symptoms can recur.
Action Steps for Mild Allergic Reactions (When Epinephrine Is Not Indicated)
For mild, localized symptoms (for example, a few hives without breathing issues, normal voice, normal behavior, no vomiting), focus on symptom relief and close observation because mild symptoms can progress.
Step-by-step
- 1) Stop exposure. Remove the suspected trigger and rinse the mouth if food exposure occurred.
- 2) Assess for progression. Re-check breathing, voice/cry, and overall behavior every few minutes.
- 3) Give an age-appropriate non-sedating antihistamine if the child can swallow and is not vomiting or having breathing difficulty, and if permitted by the child’s care plan.
- 4) Treat skin discomfort. Cool compresses can reduce itching. Keep fingernails short to reduce skin injury from scratching.
- 5) Escalate immediately if symptoms spread or new systems are involved. If hives become widespread, vomiting begins, cough/wheeze starts, or the child becomes lethargic, treat as anaphylaxis.
Special Scenarios and Practical Examples
Food reaction at a birthday party

A 7-year-old with known peanut allergy eats a cookie and says their throat feels “funny,” then starts coughing and develops hives on the face. Action: give epinephrine immediately (throat symptom + cough after known exposure), position for comfort, and arrange urgent medical evaluation. Do not wait to see if the antihistamine works.
First-time reaction to a new food at home
A 10-month-old tries egg for the first time and develops a few hives around the mouth but is breathing normally, playful, and not vomiting. Action: stop feeding, wipe the face, observe closely. If hives spread, vomiting starts, or breathing changes, give epinephrine if available/prescribed and seek emergency care. If symptoms remain mild, contact the child’s clinician for guidance and future allergy evaluation.
Insect sting on the playground
A 9-year-old is stung and within minutes develops widespread hives and wheezing. Action: remove stinger if visible quickly, give epinephrine, keep the child from walking around, and arrange urgent medical evaluation. If wheeze persists after epinephrine and the child has a prescribed bronchodilator, it can be used as an add-on, not a substitute.
Reaction at school with an allergy action plan
A student reports lip swelling and abdominal pain after lunch, then vomits. Even without wheeze, the combination of mucosal swelling + significant gut symptoms after eating suggests anaphylaxis. Action: follow the student’s plan, give epinephrine, notify emergency contacts, and document time and observed symptoms for responders.
Monitoring After Epinephrine: What to Watch For
After epinephrine, improvement may be rapid, but continued monitoring is essential. Symptoms can return as the medication wears off, or the reaction can progress despite initial improvement.
Watch for persistent or returning danger signs
- Breathing difficulty returning: cough, wheeze, hoarseness, noisy breathing.
- New or worsening swelling of lips, tongue, or face.
- Repeated vomiting, severe abdominal pain.
- Weakness, faintness, confusion, or unusual sleepiness.
- Skin becoming pale/gray, cool, or sweaty.
Expected side effects of epinephrine (often not dangerous)
- Fast heartbeat, shakiness, anxiety, headache, pale skin.
- Nausea or tremor.
These effects can be alarming but are generally temporary. They are not a reason to avoid epinephrine when anaphylaxis is suspected.
Building an Anaphylaxis-Ready Environment (Home and School)
Preparation reduces delays. The goal is not to create fear around allergens, but to create reliable routines that make the correct action easy under stress.
Home readiness checklist
- Two auto-injectors available (if prescribed), stored at room temperature and easy to access.
- Caregiver practice with a trainer device and a written action plan posted where caregivers can see it (kitchen, diaper bag, first aid kit).
- Clear labeling of the child’s allergens and typical symptoms.
- Cross-contact prevention routines: separate utensils when needed, clean surfaces, handwashing after allergen handling.
- Babysitter briefing: show where the auto-injector is, how to use it, and what symptoms mean “use it now.”
School and childcare readiness checklist

- Individualized allergy action plan on file and accessible to staff who supervise meals, recess, and field trips.
- Stocked, unlocked access to the student’s epinephrine per local policy, with backups for off-site activities.
- Role clarity: who administers medication, who contacts guardians, who meets emergency responders.
- Food handling protocols: cleaning tables, handwashing, avoiding food sharing, and managing classroom projects involving food.
- Training for substitutes and extracurricular staff (sports, clubs).
Documentation and Communication During an Event
In an emergency, clear communication prevents missed steps and helps medical teams continue care.
What to record (quick notes)
- Suspected trigger and time of exposure (if known).
- First symptoms and how they progressed.
- Time epinephrine was given and which device/dose.
- Whether a second dose was given and when.
- Other medications given (antihistamine, inhaler) and times.
How to describe symptoms clearly
Use observable facts: “wheezing and using belly muscles to breathe,” “vomited twice,” “voice became hoarse,” “hives on chest and back,” “became pale and floppy.” Avoid vague terms like “seemed off” without adding what you saw.
When It Might Not Be an Allergy (and Why You Still Act on Symptoms)
Some conditions can resemble allergic reactions: viral rashes, heat rash, contact irritation around the mouth, asthma flare without allergy, panic/hyperventilation in older children, or fainting from pain. The reason action plans emphasize epinephrine for suspected anaphylaxis is that the cost of missing true anaphylaxis is high, and epinephrine is the only medication that rapidly treats the life-threatening features. If a child has clear breathing or circulation compromise after a plausible exposure, treat first and let clinicians sort out the final diagnosis.
Practical Skills: Teaching Children to Self-Report and Self-Carry (When Appropriate)
As children grow, they can participate in their own safety. The goal is simple, age-appropriate habits.
Preschool and early elementary
- Teach them to say: “I feel sick,” “My throat feels funny,” “I can’t breathe,” “I need my allergy medicine.”
- Practice not sharing food and asking an adult before eating.
Older elementary and middle school
- Teach them to recognize early symptoms and to alert an adult immediately.
- If permitted, teach how to carry auto-injectors and when to use them, emphasizing that using it is not “getting in trouble.”
Teens
- Discuss real-life risk situations: dating, restaurants, sports, and peer pressure.
- Rehearse scripts for asking about ingredients and for telling friends what to do if symptoms start.
Mini-Reference: Symptom-to-Action Mapping
Use this as a quick mental map. Always follow the child’s prescribed allergy plan when available.
- Only a few hives/itching, child otherwise well: stop exposure, observe closely, consider antihistamine if safe.
- Hives plus vomiting or severe belly pain: treat as anaphylaxis; give epinephrine.
- Any breathing symptom (cough, wheeze, hoarse voice, throat tightness, noisy breathing): give epinephrine.
- Faintness, collapse, extreme lethargy, pale/gray color: give epinephrine and treat as anaphylaxis.
- Known allergen exposure with rapidly progressing symptoms: give epinephrine early.