Why Written Plans and Logs Matter in Real Emergencies
In homes, schools, and childcare settings, emergencies often involve multiple adults: parents, grandparents, babysitters, teachers, coaches, neighbors, and after-school staff. Even when everyone is capable and calm, details get lost: which parent to call first, which clinic the child uses, what medication is taken daily, what dose is typical, what the child is allergic to, and what “normal” looks like for that child.
Caregiver action plans, emergency contact sheets, and allergy/medication logs are simple tools that reduce confusion and speed up correct decisions. They do not replace medical advice or emergency services. They are designed to make sure the right information is available immediately, to the right person, in the right format.
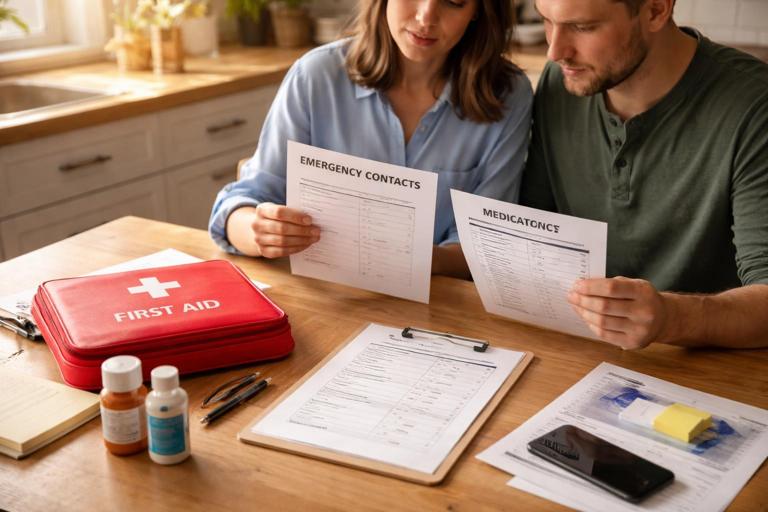
Think of these documents as “information first aid.” They help you communicate quickly and consistently with other caregivers and with professionals (school nurse, urgent care staff, paramedics) without relying on memory.
Three Core Documents and How They Work Together
1) Caregiver Action Plan (CAP)
A caregiver action plan is a one-page (or two-page) set of instructions tailored to a specific child and setting. It tells a caregiver what to do in common urgent situations for that child, who to contact, what supplies are available, and what permissions exist. It is not a medical textbook; it is a practical “if this, then that” guide.
Examples of when a CAP is useful:
- Listen to the audio with the screen off.
- Earn a certificate upon completion.
- Over 5000 courses for you to explore!
Download the app
- A child with severe allergies who attends birthday parties and after-school care.
- A child who takes daily medication and sometimes refuses it.
- A child who has a complex custody arrangement with different pickup permissions.
- A child with communication challenges who cannot reliably describe symptoms.
2) Emergency Contact Sheet (ECS)
An emergency contact sheet is a standardized list of who to call, in what order, and how to reach them. It includes backup contacts and key identifiers. It should be easy to scan in under 10 seconds.
Unlike a CAP, the ECS is not situation-specific; it is always relevant. It is the document you hand to a substitute teacher, a babysitter, or a neighbor who is helping for one afternoon.
3) Allergy/Medication Log (AML)
An allergy/medication log is a living record of allergies, current medications, and medication administration history when relevant (especially for children who receive doses at school, daycare, or by multiple caregivers). It helps prevent double-dosing, missed doses, and accidental exposure to allergens.

Depending on the child, the AML can be very short (a list of allergies and daily meds) or more detailed (dose times, changes, side effects, and prescriber details).
Design Principles: Make It Usable Under Stress
These tools only help if people can and will use them. Design for real life:
- One-page priority: Put the most critical information on the first page. If there is a second page, it should be “details.”
- Plain language: Use simple words and short sentences. Avoid medical jargon unless it is a medication name or diagnosis that must be exact.
- Big, scannable structure: Use headings, bullet points, and bold labels. Avoid long paragraphs for critical instructions.
- Consistency: Use the same format across children if you manage multiple kids (classroom, daycare). Familiar layouts reduce errors.
- Date and version: Every document should show “Last updated: ____” so caregivers know it is current.
- Permission clarity: Include who can pick up the child, who can authorize care, and any legal restrictions that affect contact.
- Privacy-aware: Share only what is needed for safety. Store securely and limit access to appropriate caregivers.
Step-by-Step: Build a Caregiver Action Plan (CAP)
Use this step-by-step process to create a CAP that is practical and specific. Aim for one page for most children; two pages if there are multiple conditions or complex logistics.
Step 1: Identify the settings and caregivers
List where the plan will be used and by whom. A plan for “home evenings” may differ from “school field trips.”
- Settings: home, school, daycare, sports, grandparents’ house, babysitter, carpool.
- Caregivers: names and roles (teacher, coach, sitter), plus their typical access to supplies (meds, phone, car).
Step 2: Define the child’s baseline and communication needs
Include what helps caregivers interpret symptoms correctly.
- Baseline notes: typical energy level, usual appetite, common benign complaints.
- Communication: preferred words/signs, sensory triggers, how the child expresses pain, whether they can state name/address.
- Comfort strategies that help cooperation: favorite distraction, preferred position, who calms them fastest.
Step 3: List the child-specific “high priority” situations
Choose the situations that are most likely or most dangerous for that child. Keep it short and relevant.
- Examples: severe allergy exposure risk, asthma flare patterns, diabetes care steps (if applicable), tendency to faint, history of complex febrile illness, medication that must not be missed.
Step 4: Write “If–Then” action blocks
Each block should include: what to look for, what to do immediately, what to monitor, and who to contact. Keep each block to 5–8 bullet points.
Example structure (template wording you can adapt):
- If you notice: (specific signs the caregiver can recognize)
- Do now: (simple actions within caregiver scope)
- Then: (next steps, including contacting parent/guardian and/or medical support)
- Bring/Share: (medications, logs, insurance card copy, action plan)
Practical example (non-medical, logistics-focused):
- If the child becomes suddenly ill during a field trip: move to a quiet supervised area; notify trip lead; check the child’s emergency contact sheet; call Parent/Guardian #1; if unreachable after 2 minutes, call Parent/Guardian #2; if transport is needed, bring the child’s medication pouch and contact sheet; document time and what was observed.
Step 5: Add logistics that prevent delays
Many emergencies become harder because of missing items or unclear permissions.
- Where medications are stored (exact location) and who has the key/code.
- Where the child’s health insurance card copy is kept (if applicable).
- Preferred clinic/pediatrician and nearest urgent care (address and phone).
- Transportation notes: who can drive, car seat location, permission for rideshare/taxi if relevant.
- Language needs: preferred language for caregivers; interpreter needs.
Step 6: Add consent and custody notes (only what is necessary)
Keep this factual and brief.
- Who can authorize emergency care if parents are unreachable.
- Who is allowed to pick up the child.
- Any restraining order or “do not release to” instruction (follow your local legal requirements; schools/daycares often have formal processes).
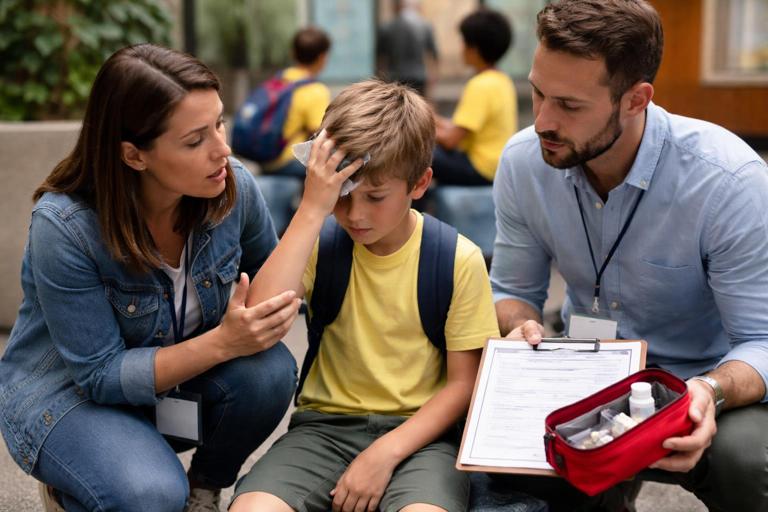
Step 7: Review with all regular caregivers
A plan is only effective if people understand it. Walk through it with:
- Babysitters and relatives
- Teachers/daycare staff (as allowed)
- Coaches/activity leaders
Ask them to point to the first three things they would do in a stressful moment. If they hesitate, simplify the plan.
Step-by-Step: Create an Emergency Contact Sheet (ECS)
The ECS should be a single page, ideally half-page, that can be posted discreetly or stored in a binder and shared quickly.
Step 1: Child identifiers
- Child’s full name and preferred name
- Date of birth
- Home address
- School/class/teacher (if relevant)
- Primary language
Step 2: Primary contacts in strict order
List contacts in the exact order you want them called. Include:
- Name, relationship, phone numbers (cell/work), and email
- Best times to reach and any “do not call at work” constraints
- Backup method (text preferred vs call)
Step 3: Backup adults who can act
Include at least two local backups who can arrive quickly.
- Names and phone numbers
- Address (if nearby)
- Pickup permission status
- Any special instructions (e.g., “has spare house key,” “has car seat base”)
Step 4: Medical contacts and preferred facilities
- Pediatrician/clinic name, phone, address
- Preferred hospital (if you have one) and nearest emergency department
- Specialist contact (if applicable)
- Pharmacy name and phone
Step 5: Insurance and documentation notes
Depending on your setting, you may include:
- Insurance provider and member ID (or note: “copy of card in backpack pocket”)
- Parent/guardian ID location if needed for pickup
Step 6: Make it easy to find and hard to lose
- Print two copies for home: one in a known kitchen/entry location, one in the first aid kit binder.
- For school/daycare: follow their policy; often it goes in the child’s file and a classroom emergency folder.
- For activities: keep a folded copy in the child’s bag in a labeled sleeve.
Step-by-Step: Build an Allergy/Medication Log (AML)
The AML prevents mistakes when more than one adult gives medication or manages food exposure. It also helps you notice patterns (missed doses, side effects, symptom changes) that can be shared with a clinician.
Step 1: Separate “Allergy List” from “Medication List”
Keep allergies and medications distinct so caregivers do not confuse them.
- Allergies: food, medication, insect, environmental; include reaction type if known (e.g., hives, vomiting) and severity notes.
- Medications: daily meds, as-needed meds, emergency meds; include exact name and form (liquid, tablet, inhaler), and where it is stored.
Step 2: Record essential medication details
For each medication, include:
- Name (generic and brand if helpful)
- Purpose (one short phrase, e.g., “daily allergy control”)
- Strength/concentration (especially for liquids)
- Usual dose and route (by mouth, inhaled, topical)
- Schedule (time windows rather than exact times if that fits your routine)
- Prescriber and pharmacy
- Start date and any planned stop date
- Known side effects for this child (if observed and confirmed)
Step 3: Add a medication administration record (MAR) section when multiple caregivers give doses
If the child receives doses at school, daycare, or between households, add a simple table to prevent double-dosing.
Date | Medication | Dose | Time given | Given by | Notes (symptoms, refused, spit up)Practical tips:
- Use a single shared notebook kept with the medication pouch, or a shared digital log if all caregivers reliably use it.
- Write immediately after giving a dose, not later.
- If a dose is refused or vomited, record what happened and when, so the next caregiver does not guess.
Step 4: Track allergy exposures and near-misses
For children with significant allergies, add a brief incident log. This is not for blame; it is for prevention.
Date | Suspected trigger | Where | What happened | Action taken | Outcome | Prevention noteExample entries:
- “Snack time: cookie shared by classmate; stopped before bite; reminder sent to teacher about food-sharing rule.”
- “Restaurant: sauce contained nuts; child did not eat; updated ‘safe foods’ list for babysitter.”
Step 5: Include expiration dates and replacement plan
Many emergency medications and some routine medications expire or need periodic replacement.
- List expiration dates in a dedicated column.
- Set a calendar reminder 30–60 days before expiration.
- Note where backups are stored (home vs school vs travel bag).
Practical Examples: What to Include (and What to Leave Out)
Example: A simple CAP for a generally healthy child
Even without chronic conditions, a CAP can focus on logistics:
- Child’s identifiers and baseline behavior
- Emergency contact order and backup pickup adults
- Where the first aid kit is and where the child’s bag is kept
- Permission notes: who can authorize care if parent unreachable
- School/daycare policy reminders: where forms are stored, who to notify
What to leave out: long descriptions of medical emergencies already covered elsewhere, or detailed treatment instructions beyond caregiver scope.
Example: A CAP for a child with allergies and daily medication
Keep the CAP focused on recognition cues and logistics:
- Known allergens and strict avoidance rules (e.g., “no food sharing”)
- Location of emergency medication pouch and who carries it
- Clear contact order and preferred hospital
- Where the allergy/medication log is kept and how to document exposures
- Field trip checklist: meds packed, expiration checked, trained adult assigned
What to leave out: repeating the full action steps for anaphylaxis if those steps are already in a separate standardized plan provided by a clinician/school. Instead, reference where that plan is stored and ensure it is attached.
Example: A custody-sensitive ECS
When family situations are complex, clarity prevents conflict and delays:
- List the legal guardians and their contact order
- List approved pickup adults
- Provide a brief “do not release to” instruction only if formally documented and required by your institution’s policy
- Include a note: “If there is disagreement between adults, follow the contact order and school/daycare policy; do not mediate.”
Storage, Access, and Privacy: Getting the Balance Right
These documents must be accessible in an emergency, but not casually visible to everyone.
Home
- Keep a printed ECS in a consistent location (inside a cabinet door, in a labeled binder, or with the first aid kit).
- Keep the CAP and AML in a “Child Health” folder that any caregiver can find quickly.
- If you use a digital version, ensure at least one printed copy exists in case phones are unavailable.

School/Daycare
- Ask where emergency forms are stored and who can access them quickly (front office, nurse, classroom emergency folder).
- Provide updated copies whenever medications change.
- Confirm the policy for field trips and extracurriculars (who carries meds, where forms travel).
On the go (sports, travel, babysitters)
- Use a sealed pouch with: ECS, key medical notes, and the minimum necessary medication information.
- For babysitters, provide a “quick start” sheet: where you are, when you return, and the top three contacts.
Maintenance Routine: Keep Documents Accurate
Outdated information can be worse than none. Use a simple maintenance schedule.
Update triggers (update immediately when any of these change)
- New medication, dose change, or stopped medication
- New allergy or change in reaction severity
- New pediatrician, pharmacy, or insurance
- Address change, school change, or caregiver change
- Custody/pickup permission change
Scheduled reviews
- Monthly: check medication expiration dates and refill status.
- Every 3–6 months: review contact numbers and backup adults.
- Before each new school term/season: reissue copies to school, coaches, and caregivers.
Version control
Put “Last updated” at the top of each document. If you distribute multiple copies, add a version number (e.g., “v3”). When you update, collect and shred old copies when possible.
Training Caregivers to Use the Documents (Mini-Drills)
A plan that sits in a folder is not a plan; it is paperwork. Build familiarity with short, realistic practice.
Two-minute orientation for new caregivers
- Show the ECS and point to the call order.
- Show where the CAP is stored and what it covers.
- Show where medications are stored and how to access them (keys/codes).
- Explain documentation expectations: “If you give any medication or there is any exposure/incident, write it in the log immediately.”
Five-minute scenario drill (once per season)
Pick one scenario relevant to your child and setting and practice the information flow, not the medical technique.
- Who calls whom?
- What document is grabbed first?
- What items travel with the child (med pouch, ECS, insurance copy)?
- Who stays with the child and who communicates?
Templates You Can Copy and Customize
Caregiver Action Plan (CAP) skeleton
Child: __________ DOB: __________ Preferred name: __________ Last updated: __________ (v__)
Baseline/communication notes: ______________________________________________
High-priority notes (child-specific): _______________________________________
Emergency contact order: (See attached ECS)
Medication location/access: ________________________________________________
Preferred clinic/hospital: _________________________________________________
Permissions/pickup notes: _________________________________________________
Situation blocks:
1) If you notice: __________________ Do now: __________________ Then: __________________
2) If you notice: __________________ Do now: __________________ Then: __________________
3) If you notice: __________________ Do now: __________________ Then: __________________Emergency Contact Sheet (ECS) skeleton
Child: __________ DOB: __________ Address: __________________ Last updated: __________
Call order:
1) __________ (__________) Cell: __________ Work: __________
2) __________ (__________) Cell: __________ Work: __________
Backup pickup adults:
A) __________ Phone: __________ Address: __________ Pickup: Yes/No
B) __________ Phone: __________ Address: __________ Pickup: Yes/No
Medical:
Pediatrician/Clinic: __________ Phone: __________ Address: __________
Pharmacy: __________ Phone: __________
Preferred hospital/ED: __________ Address: __________ Phone: __________Allergy/Medication Log (AML) skeleton
Allergies (trigger | typical reaction | severity notes | last updated):
- ________________________________________________
Current medications (name | purpose | strength | dose | schedule | prescriber | pharmacy | expires):
- ________________________________________________
Medication administration record (if needed):
Date | Medication | Dose | Time | Given by | Notes
____ | _________ | ____ | ____ | ________ | __________________
Exposure/near-miss log (optional):
Date | Trigger | Where | What happened | Action taken | Outcome | Prevention note
____ | _______ | _____ | _____________ | ____________ | _______ | ______________